Did you know seasonal depression affects about two percent of people without a pre-existing mental health condition and 20 percent of people already diagnosed with a depressive disorder? Seasonal depression significantly reduces productivity and mood, and students and teachers with seasonal depression struggle with learning and teaching. Awareness about the disorder is imperative among the educational community.
According to the National Institute of Mental Health, seasonal depression occurs due to low dopamine and high melatonin levels. Dopamine is produced by your brain when you are exposed to sunlight or vitamin D. Some people also have vitamin D deficiency throughout the year, but it becomes more prevalent in winter because there is less sun.
Vitamin D is produced by people’s bodies when exposed to the sun. In winter, the sky is usually overcast, and if it is cold or snowing, people usually remain indoors. In addition, during the winter, days shorten due to the occupied hemisphere tilting away from the sun. All of these factors lead to a lack of or reduced exposure to direct or indirect sunlight. Being exposed to less sunlight leads to lower dopamine and increased melatonin levels.
Seasonal depression is different from a depressive disorder. It is caused by a lack of sunlight, while a depressive disorder can be caused by a stressful life, grief, isolation, trauma, etc. or even a chemical imbalance.
Seasonal Affective Disorder (SAD) is a type of depression that happens during the fall and winter months. Although it can occur during the spring and summer months it is less common compared to the darker, colder months.
Despite there not being a clear cause, some theories have been established as to why our body experiences this. One theory is that during days with less sunlight, the body overproduces melatonin, causing people to sleep more or eat more to restore their energy. It is also thought that people with SAD have less serotonin, or the circadian rhythm in the body has been desynchronized.
Not everyone will experience the same symptoms of SAD. Symptoms can include being increasingly irritable, unusually sad, losing interest in activities that you would normally enjoy, changes in habits (overeating), being tired or sleeping a lot, feeling hopeless or worthless and thoughts of death or suicide. SAD can affect everyone, but it most often develops in people in their early 20s.
When diagnosing SAD, healthcare professionals will rule out other medical issues or conditions that have the same symptoms. They will have to make sure that there is nothing else that could cause these symptoms, such as something emotional or physical. The biggest thing to look for when diagnosing SAD is having two seasons where a person is feeling depressed for at least two years.
Once a person is diagnosed with SAD, a doctor will recommend a few treatments such as light therapy or phototherapy. Light therapy involves a special kind of light that simulates daylight; a person is to sit in front of the light for 30 minutes or more in the morning and occasionally in the afternoon. This can help improve symptoms within a couple of days or weeks depending on the severity of the condition.

In addition, some doctors can prescribe vitamin D pills to people with a vitamin D deficiency. Some people also benefit from Cognitive Behavioral therapy (CBT). This treatment focuses on helping patients combat negative thoughts and feelings.
In more severe cases, a person can be treated with antidepressants to help balance serotonin and other neurotransmitters that impact a person’s mood.
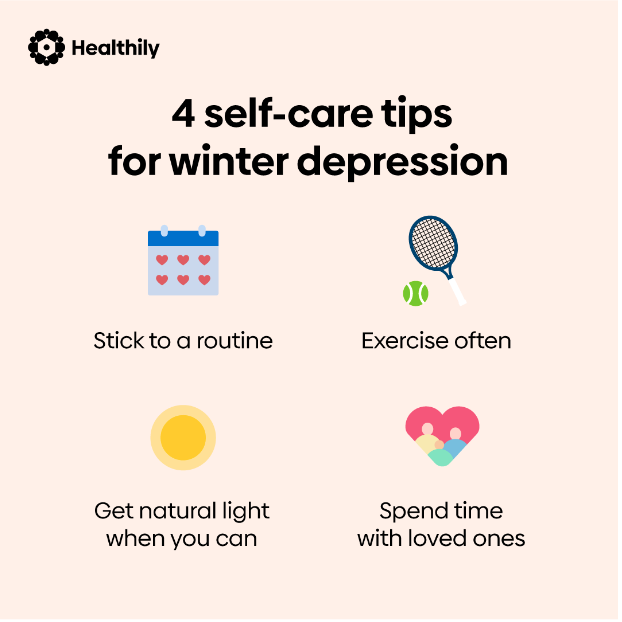
It is also important to make a routine to help with treatment, making a schedule for meals, sleep and treatment or therapy that helps improve your SAD. SAD disrupts the body and mind’s sense of stability, making it important to have a routine.
Seasonal depression is a widespread phenomenon that affects a variety of people. It is not something we can fight directly; however, by supporting those who experience it and showing that we care, we help make the world a better place.