Every second of the day, your body is fighting a war. And yet, you never feel or see it. Your immune system is locked in a constant battle against pathogens and foreign substances that enter your body, keeping you healthy. But have you ever wondered how immune cells can distinguish a specific pathogen from the millions of cells in your body?
This is the primary task of the Major Histocompatibility Complex (MHC). The MHC is an essential part of the immune system that allows our immune cells to identify our body’s cells from foreign cells.
A Deep Dive Into The MHC
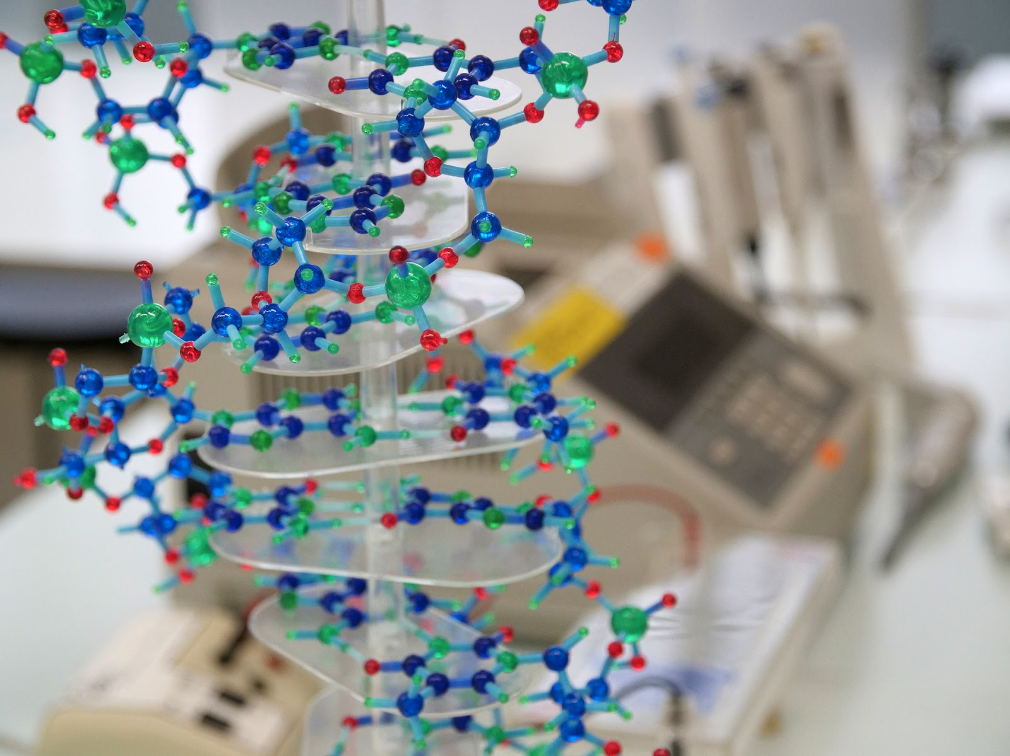
The MHC is a set of cell-surface proteins that, according to the Gale Encyclopedia of Genetic Disorders, “are present on the surface of most of the body’s cells and are important in helping the immune system distinguish ‘self’ from ‘non-self.’”
MHC molecules bind to peptide fragments, which are little bits of proteins that are created by pathogens and our cells. They display them on the cell surface for recognition by T cells, or immune cells that can kill cells and trigger an immune response.
MHC molecules are coded by the Human Leukocyte Antigen (HLA) complex, a gene group that contains the most polymorphic genes in the human genome — genes that can code for multiple variations of proteins. HLA genes are also co-dominantly inherited, meaning that a person expresses alleles from both parents. This allows every person to have a unique set of MHC molecules combined from both parents, which helps the immune system differentiate “self” from “non-self.”
“Self” Versus “Non-self”
Our cells would not be able to recognize our own body cells from foreign cells if it were not for the MHC. The MHC presents all cell production for T cells to determine if any abnormal proteins are being made. The MHC 1 on our body cells presents self-peptides, or peptides that our cells normally create. If peptides unlike these self-peptides are present, the cytotoxic T cells– cells that can kill our body cells– roaming our body and scanning our cells will know that something is wrong and will kill the cells.
The MHC molecules on one individual’s cells are unique to them. Our body has its own unique “fingerprint” to distinguish itself from a foreign cell, similar to how we can unlock our phones with our unique face or fingerprint. The histocompatibility, or the similarity of the MHC between a donor and recipient, plays a large role in the acceptance or rejection of a transplant.
Transplanted organs from donors have different MHC molecules than their recipients. If the T cells of one individual recognize the other individual’s MHC molecules as foreign, they will initiate an immune response. This is a great example of how the MHC determines “self” versus “non-self.” Think of it like a factory in which the MHC are the products and the T cells are the factory inspectors who will sort out any products with deformities.
The Types of MHC
There are two major types of MHC: Class I and Class II. Lesser known is the MHC Class III. Class I MHC molecules are found on the membrane of almost every one of our bodily cells. Class II MHC molecules are only found on the membrane of our immune cells, like macrophages, dendritic cells and lymphocytes. Class III MHC molecules are proteins that serve various different functions in the immune system.
MHC I
MHC I molecules’ main goal is to bind to cytotoxic T cells, helping them recognize any harmful body cells. These MHC I molecules present the peptide fragments of the proteins our cells are creating, allowing the cytotoxic T cells to detect infected or abnormal body cells. The MHC I and peptide complexes are anchored to the cell membrane. There, the MHC I and peptide complexes can be recognized by the cytotoxic T cell’s receptor (TRC).
The TCR will check the peptide attached to the MHC I. If it recognizes a foreign peptide antigen in the MHC I molecule, it will know that the cell is infected or cancerous and kill it. It will not, however, recognize the self-peptides bound to MHC I. This ensures that our immune cells will not attack our healthy cells.
MHC II
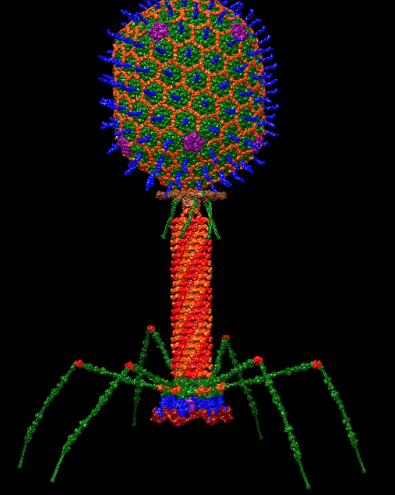
Unlike MHC I, which is present in almost all cells, MHC Class II can only be found on immune cells. MHC II binds to helper T cells, which in turn trigger an immune response. MHC II presents antigens from pathogens– peptides from disease-causing germs– that are engulfed by specific immune cells called antigen-presenting cells in a process known as phagocytosis.
These antigens are attached to MHC II molecules and transported to the cell membrane of the antigen-presenting cell. Helper T cells then bind to the MHC II and are activated when they see the antigen in the MHC II. They mount an immune response and rally immune cells to fight off the pathogen. This is the response in action when you feel sick.
MHC III
Not much is known about MHC Class III other than that it is a group of proteins containing many signaling molecules involved in inflammation. According to the National Library of Medicine, “[MHC Class III] contains 61 genes and is the most gene-dense region of the human genome.” But MHC III is poorly defined both structurally and functionally. It does not present antigens or have a clear function in the immune response like MHC classes I and II. Some examples of MHC Class III are enzymes, complement proteins which help kill bacteria and cytokines which signal your immune cells.
The Similarities and Differences of MHC I and MHC II
The main difference between the two MHC classes is that MHC I serves as a window into our body cells, but it does not actively decide whether they are a threat or not. That decision is left up to the cytotoxic T cells. MHC II serves as a flag post that waves around antigens to alert the immune system of intruders and they tell the helper T cells to kick off an immune response.
Though both MHC classes do have similarities, according to LaboratoryInfo, a blog by a group of doctors, “[Both MHC classes are] surface antigens expressed on the membrane of the cell. They are both antigens found on T cells. They are both involved in eliciting immune responses to fight foreign antigens.”
Without both MHC I and MHC II, our immune system would not function as it would not be able to recognize if something foreign was in our body, allowing pathogens and abnormal body cells to run amok.
The Future of MHC in Medicine
Transplants’ successes are extremely reliant on how our bodies respond to a donor’s MHC I molecules. They are sometimes rejected by our immune system; but with new advances in medicine, donors’ organs and grafts can be modified to match the “self” of recipients. Technology like Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) used in DNA editing has been used to change the HLA genes of a donor to match the recipient’s MHC, reducing the probability of rejection by the recipient.
If we can figure out how to accurately change which MHC molecules are presented on our cells, it will not matter who donated organs, as there will be no chance of rejection.
According to Dr. Sung Yoon Choo, a pathologist with over 21 years of experience, “The benefits of HLA matching are well established in kidney transplantation. There is a clear relationship between the degree of HLA matching and kidney graft survival in transplants from living-related donors.” In simpler terms, organs from closely related donors like siblings that are HLA-identical or similar have a higher chance of a successful transplant.
Our bodies depend on these numerous cell-surface proteins of MHC I, II and III to keep our immune systems from attacking our cells. There is still so much to discover about the MHC and many more possible ways to utilize it in future medicinal advancements. Without the MHC, our immune system would fail and kill us from the inside out.