An assassin rooted in our own DNA, cancer has remained one of the most consistent threats to human health throughout human history. Today, modern medical advancements have opened multiple options for cancer treatment, saving lives and futures. The foundations of cancer treatment can be separated into four distinct pillars: surgery, chemotherapy, radiation therapy and –more recently added– immunotherapy. Immunotherapy, which utilizes a person’s immune system to fight against their cancer cells, has taken off in the 21st century, bringing revolutionary treatments that can shrink or even eradicate cancerous tumors. One of the newest and most promising immunotherapy treatments against blood cancer is Chimeric Antigen Receptor (CAR) T-Cell Therapy, a cutting-edge, cell-based gene therapy that has sparked excitement among researchers and oncologists.
What is CAR T-Cell Therapy?
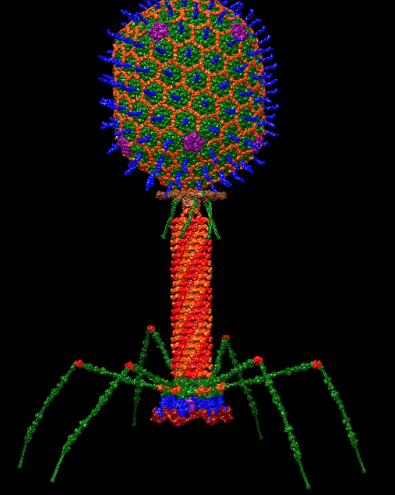
Chimeric Antigen Receptor T-Cell Therapy (CAR T-Cell Therapy) is a type of immunotherapy where T-cells are taken from the patient’s blood and modified in a lab to fight the patient’s cancer. T-cells are your body’s fighters; they are white blood cells that express a receptor that can recognize antigens. Antigens are small bits of proteins from pathogens or tumors that our body cells display when infected. If a T-cell sees an antigen on a cell, it will kill it.
The relationship between a T-cell and an antigen is similar to a lock and key: only a specific key, or receptor on a T-cell, binds to a particular antigen. This relationship is how our immune system builds immunity and ensures that we don’t kill our healthy body cells.
Our body is usually proficient in making and specifying T-cells for different antigens, but this system is not foolproof. Cancer cells can evade the immune system’s surveillance by restricting antigen recognition. This causes the body to recognize the tumor’s antigens as normal and T-cells don’t fight the cancer. This is where CAR T-Cell Therapy can be used to treat the hidden cancer.
How Does CAR T-Cell Therapy Work?
CAR T-cells have receptors that are genetically engineered in a laboratory to have new receptors specifically coded for the antigens on cancer cells. CAR T-cells are only able to detect a single cancer antigen for a specific person, as different cancers have different antigens. This means that CAR T-cells can only fight one type of cancer, usually blood cancer.
There are three main steps in CAR T-Cell Therapy. First, white blood cells are removed from the patient’s blood through a procedure called leukapheresis. From these white blood cells, the patient’s T-cells are separated. Then, the T-cells are sent to a lab where the specific chimeric antigen receptor gene is added to the T-cells’ DNA, making them CAR T-cells. The CAR gene allows the T-cells to produce proteins on their surface called chimeric antigen receptors (CARs). The CARs recognize and bind the antigens on the cancer cells. The new CAR T-cells are then grown in a lab and multiplied to the number needed for the therapy. Finally, the CAR T-cells are infused back into the patient’s blood, where they start to bind with the cancerous cells, all while multiplying. According to Renier J. Brentjens, a doctor at Memorial Sloan Kettering Cancer Center in New York City, CAR T cells are like “giving patients a living drug,” created from the patient’s immune cells.
The Possible Side Effects of CAR T-Cell Therapy
Like all cancer treatments, CAR T-Cell Therapy can have serious side effects, such as the mass death of B-cells, infections, brain swelling and serious neurological effects. One of the most frequent side effects is cytokine release syndrome (CRS). Cytokines are chemical messengers that are released by T-cells which help direct the immune system. CRS occurs when too many cytokines are produced. This is common in CAR T-cell Therapy, as millions of engineered T-cells are introduced to the body. CRS causes extremely high fevers and sometimes low blood pressure.
CAR T-Cell Therapy can also result in dying B-cells. B-cells are a type of white blood cell that produce antibodies and present antigens on their surfaces that trigger an immune response. Sometimes, the receptor on the CAR T-cells can target the antigens on the healthy B-cells, killing them and dropping the levels of antibodies in the blood to dangerously low levels, leaving the patient at high risk of infection.
There may also be serious effects on the nervous system, such as brain swelling and inflammation, which can be dangerous if not treated quickly. Other symptoms include headaches, confusion, agitation, seizures, tremors, loss of balance and trouble speaking or understanding.
What is The Future of CAR T-Cell Therapy?
The first CAR T-Cell Therapy was approved by the Food and Drug Administration (FDA) in 2017. Since then, six CAR T-Cell Therapies have been approved. The approved CAR T-cell therapies are Tisagenlecleucel (Kymriah), Axicabtagene (Yescarta), Brexucabtagene autoleucel (Tecartus), Lisocabtagene maraleucel (Breyanzi), Idecabtagene vicleucel (Abecma) and Ciltacabtegene autoleucel (Carvykti). All of these therapies are used to treat blood cancers like leukemia, lymphomas and multiple myeloma.
According to James Kochenderfer, a doctor of The National Cancer Institute’s (NCI) Center for Cancer Research (CCR), advanced aggressive lymphomas “were virtually untreatable” before the development of CAR T-Cell Therapy. Now, “CAR T cells [have] become a frequently used therapy for several types of lymphoma” that are “incredibly successful.”
Today, Steven Rosenberg, the chief of the Surgery Branch in NCI’s CCR says that “[CAR T cells] are now widely available in the United States and other countries and have become a standard treatment for patients with aggressive lymphomas,” and that, “they have become a part of modern medicine.” Research into CAR T-cell Therapy is continuing at a rapid pace, with hundreds of ongoing clinical trials, leading to new and more advanced immunotherapy cancer treatments.